To reduce the spread of COVID-19, public health experts have closed or restricted certain high-risk settings. We often are questioned why specific settings are designated as high risk. The evidence that some settings are particularly risky comes from several sources, including laboratory studies showing the conditions needed for virus to spread, reports of outbreaks, and special epidemiologic studies. This is a summary of evidence suggesting that certain settings are especially likely to promote the spread of COVID-19.
Restaurants
Restaurants – especially indoor dining – have been identified through studies of various types as high-risk settings for the spread of SARS-CoV-2, the virus that causes COVID-19. This is not surprising, because at restaurants customers are not wearing masks, are talking, often at high volume, and are in close contact for prolonged periods of time. Indoor dining further raises the risk by being an enclosed space. In Minnesota, as of December 26, 2020, more than 200 outbreaks of COVID-19 had been traced to restaurants and food service establishments. Aside from congregate health care settings, more outbreaks have occurred in restaurants than in any other setting. Data from the Washington State Department of Health show that outbreaks at restaurants and bars accounted for more total cases and more cases per outbreak than outbreaks in any other non-health care setting. Even spacing tables farther than six feet is not guaranteed to prevent spread. In a South Korean restaurant an outbreak was traced to diners sitting more than 20 feet apart.
Special epidemiologic studies reinforced the evidence that restaurants are especially high-risk settings. A CDC study found that the going to a restaurant, bar, or coffee shop was the highest-risk community exposure for COVID-19. The figure below shows that adults with COVID-19 were about twice as likely (adjusted odds ratio 1.9) to have visited a restaurant in the 14 days before becoming sick as those without COVID-19. JPMorgan analyzed data from 30 million Chase cardholders and Johns Hopkins University’s case tracker and found that the “level of spending in restaurants three weeks ago was the strongest predictor of the rise in new virus cases over the subsequent three weeks…Conversely, higher spending at supermarkets predicted a slower spread of the virus.” Finally, a study by researchers at Yale University found that policies closing restaurants consistently predicted lower growth in fatality four and six weeks later.
Figure 1: Adjusted odds ratio (aOR) and 95% confidence intervals for community exposures associated with confirmed COVID-19 among symptomatic adults aged ≥18 years (N=314) — United States, July 1–29, 2020.
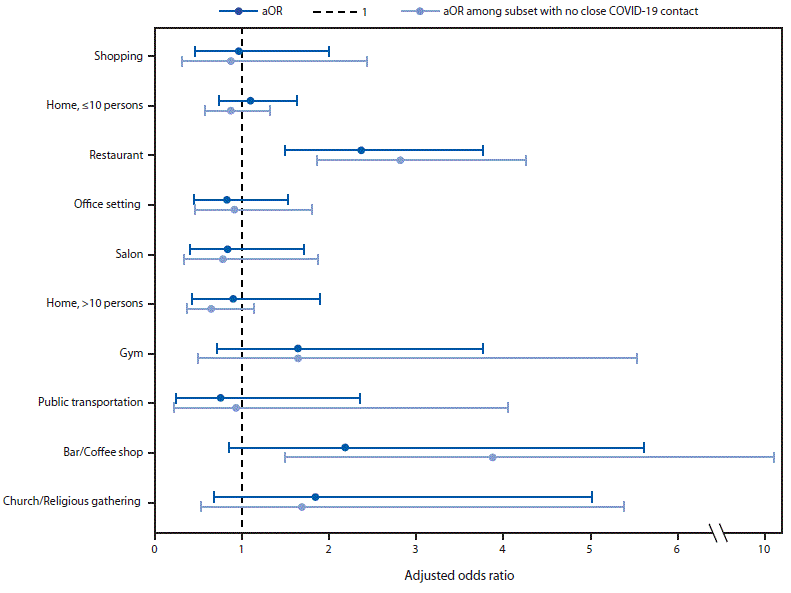
Figure 2: Reopening full-service restaurants has the largest predicted impact on infections, due to the large number of restaurants as well as their high visit densities and long dwell times.
Catered Events
Catered events, such as weddings and funerals, are occasions for friends and family to gather. Typically, guests spend several hours mingling with others outside their households. Masks are removed to eat, increasing the risk of spreading COVID-19.
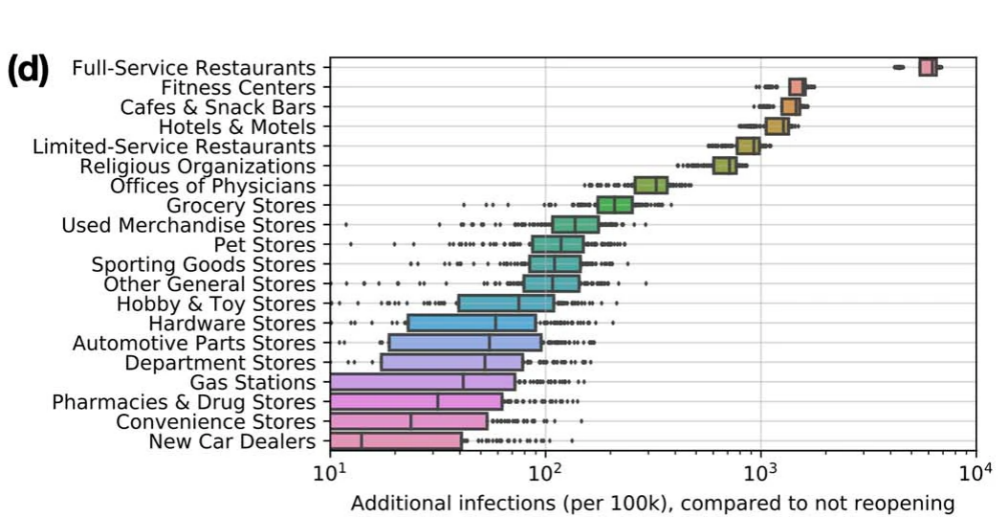
Unfortunately, many large outbreaks have been traced to weddings, funerals, and other catered events. For example, an indoor wedding in Maine in August led to multiple outbreaks. As seen in the figure below, eventually 177 cases were epidemiologically linked to the 55-person wedding. Outbreaks at a long-term care facility and a correctional facility were eventually linked back to the same wedding. Seven people required hospitalization and 7 people died. A funeral in Georgia in March became a super-spreader event. The Rose Garden event at the White House to announce the nomination of Amy Coney Barrett to the Supreme Court led to at least 12 people testing positive for COVID-19.
Figure 3: Distribution of COVID-19 cases (N=177) linked to a rural wedding reception, by date of onset or test — Maine, August 7–September 14, 2020.
Indoor gaming facilities
Patrons typically spend many consecutive hours in gaming facilities, such as casinos, and transmission of SARS-CoV2, the virus that causes COVID-19, increases with time spent exposed to the virus. In addition, some activities that take place in gaming facilities, such as table games in casinos, require close contact. County records in San Diego demonstrate that at least 638 cases of COVID-19 have been linked to seven casinos. This spread occurred despite the fact that social distancing, symptom screening, enhanced cleaning and mask wearing were taking place.
Theaters
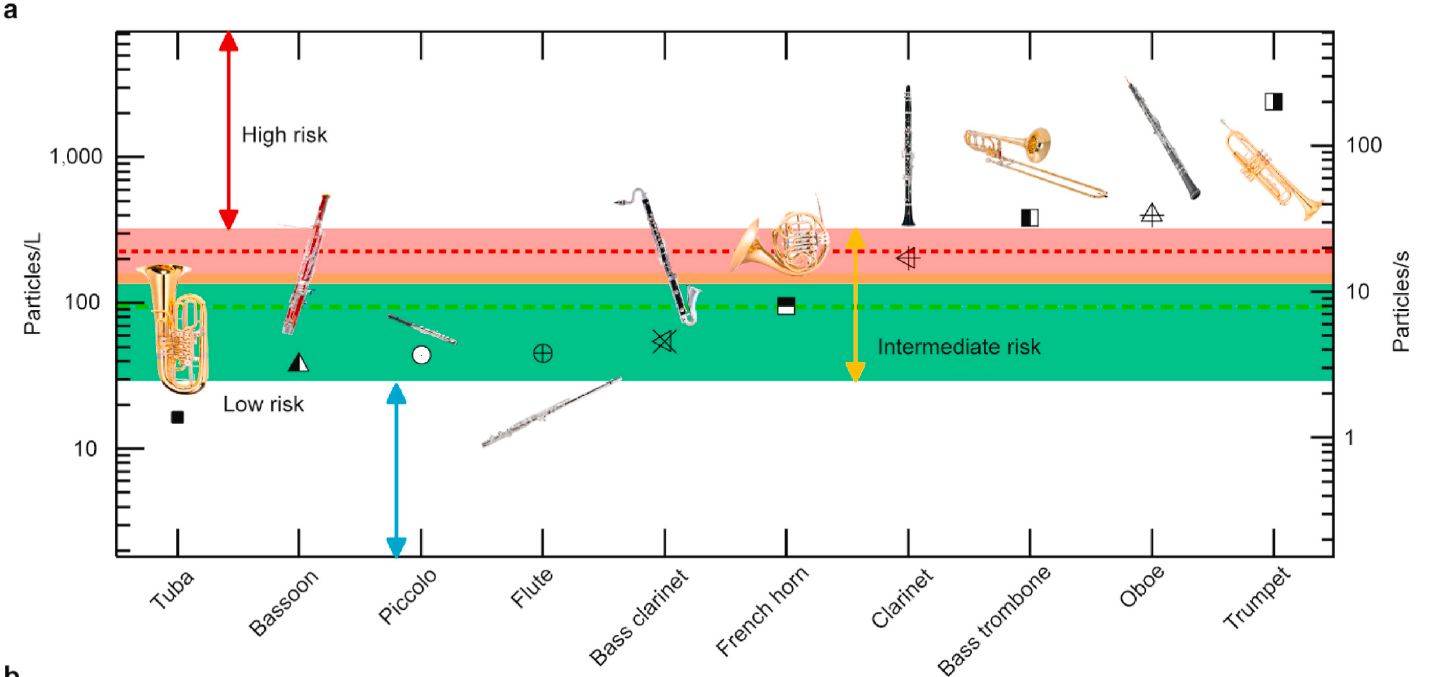
Theater performances can create favorable environments for spreading COVID-19. Audiences are commonly from many different households spending time together for extended periods of time, increasing risk of exposure to SARS-CoV2 and increasing the risk of becoming infected. In addition, during live events theater performers typically cannot distance or wear masks. Speaking loudly, singing, and playing certain instruments are all also associated with increased risk of transmission. For example, as shown in the graphic below, the University of Minnesota measured aerosol concentrations levels at the outlets of 10 orchestra instruments. The green and red dashed lines mark the aerosol concentrations of breathing and speaking, respectively. Trumpet, oboe, clarinet and trombone all exhibited higher aerosol production than either breathing or singing, which may correlate with increased risk of transmission.
Several outbreaks have been traced to theaters. An investigation of epidemiologic links in Japan from January until April found that 11% of clusters were related to live music events. The largest non-healthcare cluster observed was linked to a live music concert. Another live musical performance in Japan over the summer led to 37 positive cases among performers, staff and audience members. While some theaters are not musical in nature, there are similarities in performers singing and projecting their voices.
Figure 4: Aerosol concentration levels measured at the outlets of 10 orchestra instruments. Such levels are averaged across different dynamic levels, articulation patterns, and individuals. The green and red dashed lines mark the concentrations of breathing and speaking averaged over all participants, respectively.
Religious Gatherings
Inherent to religious gatherings are many of the factors known to lead to spread of SARS-CoV2. They usually occur indoors, often in crowds where friends and family mingle. Ceremonies, such as weddings and funerals, typically bring people in close contact with hugging and crying. Singing and chanting leads to increased spread as well.
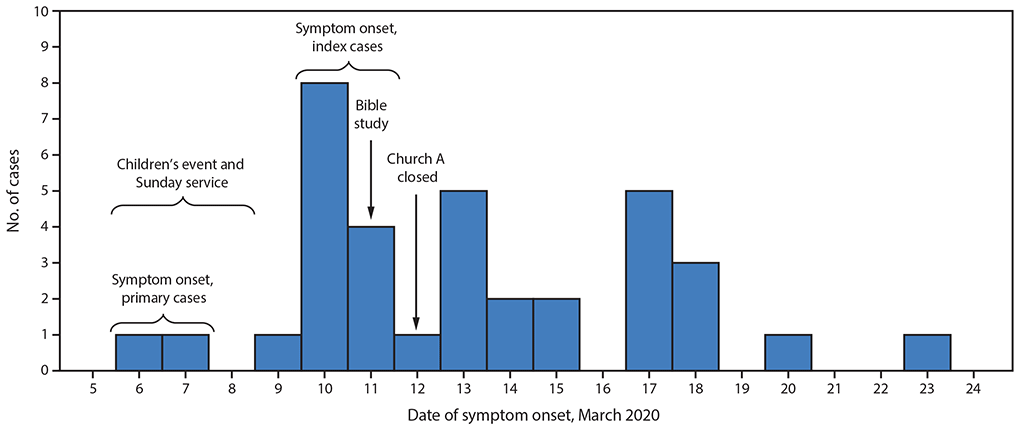
One of the first large outbreaks in South Korea was traced back to a church service. In Arkansas, 35 church attendees developed COVID-19 after attending church with two people who tested positive. Three people ultimately died of the disease. The figure below exhibits the date of symptom onset of those 35 people. Churchgoers continued to develop symptoms 11 days after the church was closed. Smaller family gatherings for holidays similarly has led to clusters.
Figure 5: Date of symptom onset among persons with laboratory-confirmed cases of COVID-19 (N=35) who attended March 6–11 church A events — Arkansas, March 6–23, 2020.
Indoor Sports
Known risk factors for COVID-19 include spending prolonged amounts of time in close contact with others. Breathing heavily likely further increases risk, while mitigation measures such as wearing masks are often not possible while playing sports.
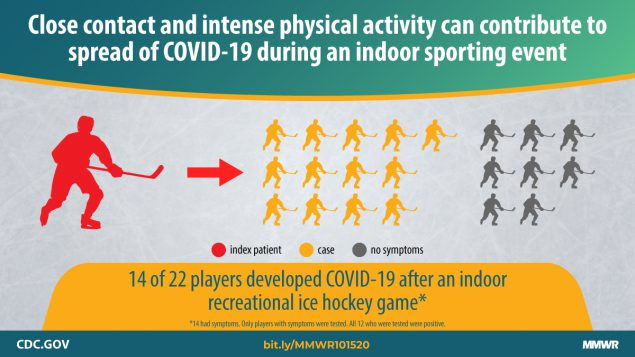
Multiple outbreaks of COVID-19 have been traced back to sports. Ice hockey is particularly high risk, possibly due to the unique environment of an indoor ice rink. Multiple outbreaks have been traced to hockey games. Other sports and classes have led to outbreaks as well, including a large outbreak traced back to aerobic dance classes in South Korea.
Gyms
Like indoor sports, gym settings often include a large number of people breathing heavily near each other. A cluster of 5 cases was identified at a squash facility in Slovenia, with indirect transmission noted to have occurred. As shown in the figure below, a modelling study of 10 large U.S. cities, including Philadelphia, demonstrated that opening fitness centers would lead to the most new infections of COVID-19 after full service restaurants. The researchers were able to demonstrate reducing maximum occupancy could cause a disproportionately large reduction in infections. For example, in Chicago, reducing occupancy to 20% of the maximum reduced infections by more than 80%, while only losing 42% of visits. Another study of social distancing restrictions imposed in different counties found that gym closures were followed by a reduction in COVID-19 fatalities 4- to 6-weeks later.