Protecting vulnerable populations
Some residents of Philadelphia are at greater risk for infection or for severe disease than others. Members of racial and ethnic minorities have higher rates of recognized infection and severe infection than Caucasians, likely related to longstanding social disadvantage. People who live in congregate settings are at greater risk for infection, and those who are elderly or have chronic medical conditions are greater risk for severe disease if infected. In Phase 2, Philadelphia will emphasize protections for these disproportionately vulnerable populations.
Racial and ethnic minorities
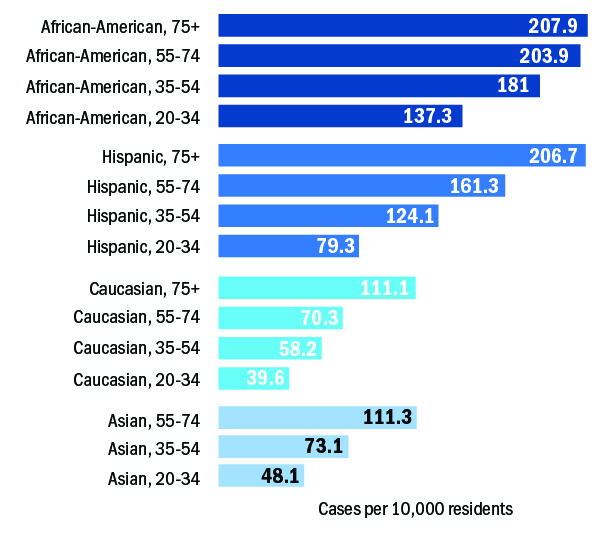
Forty-five percent of people with confirmed infection were known to be African American, 15 percent were Caucasian, 9 percent were Hispanic, 4 percent were Asian, and 23 percent were of unknown race. Rates of recognized infection rose with age, but as shown below, at any age, African Americans and Hispanics were more likely than Caucasians or Asians to have confirmed infection. Mortality rates varied by race, with higher mortality rates among African Americans (9.4 per 10,000 residents) than Caucasians (6.3 per 10,000).
In response, the Department of Public Health will develop and release a COVID-19 racial equity plan that will include actions to address:
- Improving completeness of surveillance data;
- Access to testing;
- Community outreach;
- Addressing chronic health conditions that increase the severe COVID-19 disease;
- Protecting essential workers;
- Preventing community spread; and
- Preventing spread in congregate settings.
Residents of long-term care facilities
Long-term care residents are at extremely high risk of developing severe illness from COVID-19 because they live in congregate settings and because of their age and chronic health conditions.
Ill staff and visitors are the most likely sources to spread disease into these facilities. In order to mitigate these risks, the following steps will be taken to prevent introduction of the virus into these facilities and to prevent spread within the facilities if introduced:
- Provision of ample personal protective equipment;
- Requiring masking by staff at all times (universal masking);
- Provision of COVID-19 testing supplies and rapid testing equipment to nursing homes for quick diagnosis of COVID-19 in residents or staff;
- Enforcement of restrictions on visitors and on residents leaving the facilities;
- Screening of nursing home staff at the beginning and end of each shift for fever (with temperature checks) and symptoms consistent with COVID-19;
- Testing of all symptomatic staff and, if cases are detected, testing of asymptomatic staff;
- Promotion of liberal, non-punitive sick leave policies for staff and strongly discouraging staff from working while ill;
- Screening of residents every eight hours for fever and symptoms consistent with COVID-19;
- Immediate isolation and testing of all symptomatic residents and their roommates and, if cases are detected, testing of asymptomatic residents;
- Testing of all new admissions for COVID-19 prior to transfer from acute care hospitals, and isolation precautions for 14 days following admission;
- Cohorting and other infection control actions to prevent spread when cases are detected;
- Use of serologic screening of residents and staff as appropriate to assess risk and guide cohorting; and
- Continued enforcement of restrictions on group activities, and strict enforcement of social distancing, universal masking, and enhanced hand and environmental hygiene as these activities are gradually allowed to resume.
More generally, the Department of Public Health will foster relationships between local hospitals and nursing homes, so that the expertise, staff capacity, and resources available in hospitals can support nursing homes’ infection control actions.
Other congregate settings
The Department of Public Health, in conjunction with other City and Commonwealth agencies, will work with other congregate settings, such as homeless shelters, jails, and residential psychiatric and drug and alcohol treatment facilities that house medically vulnerable people to put appropriate protections in place to reduce the likelihood that COVID-19 will be introduced into facilities and prevent spread within the facilities. In addition to congregate living settings, certain work settings maybe at higher risk for spread of virus.
When infection clusters occur in high-risk living settings or work settings. The Department of Public Health will continue to work directly with the people managing these settings to prevent, respond to, and limit these outbreaks. This will include providing personal-protective equipment, offering guidance and training on infection control, testing clients and/or staff, and advising on “cohorting” (separating) infected and uninfected clients and/or staff.
Testing of people for presence of antibodies (“serologic testing”) has recently become available and studies that help interpretation of the results of these tests are being published. COVID-19 antibodies appear to be a good marker for past infection and probably indicate protection, at least temporarily, against recurrent infection. The Department of Public Health will conduct antibody testing in some high-risk settings to assess the value of this testing to outbreak control, as well as the value to Philadelphians more broadly.